In a recent post I said; “my homoeopath is based on Alderney (they are allowed to market the more heavily proven -stronger-, remedies on/from the islands, I suspect her majesty might use some of the islands’ products)”: https://forum.5filters.info/t/more-than-5-000-licences-for-medicinal-cannabis-have-been-handed-out-by-the-states-of-guernsey-in-18-months-new-figures-have-revealed/3103
Vibrational Medicine
"the notion that a “little bit” of something cures is not the principle by which it works…both proving and potentising (the former for “remedies” the latter for “essences” ), are techniques whereby naturally pure (rather than “purified”), water (molecules), are increased in their tendency to cohere, or “imprinted” (the technique used imparting extra electro-magnetic energy either by exposure to sun/moonlight* or succussion), and to remain in the state of dynamic-tension that is the “fingerprint” of the substance to which they are exposed… Pls. see the work of #DrViktorSchauberger #DrMasaruEmoto #DrEdwardBach
*Sun for flowers Moon for crystals (the exposure times and periods also differ).
“Masaru’s work became increasingly subtle/esoteric…personally I prefer to stick to a more Schaubergian approach…water in natural systems spirals (in which direction is dependent on the hemisphere), …increasing coherence (and purity for the most part), but tap water gets pumped and its coherence destroyed (remember this is coherence in molecular clustering -sub-molecular effects are not the issue as such-), this can be seen by employing Masaru’s technique of electron-microscopy comparatively…when spirallic flow is reintroduced the molecules cohere again.”
Lets us consider what the homoeopaths and essence makers (practitioners of vibrational medicine), claim re: the interaction between these (claimed), “coherence-s” and the human endocrine system, briefly…; “that the human endocrine system whose management is via the nexus points on the susumna (spinal column), including both the pituitary and pineal glands, is like an interactive (important principle), radio antenna. It is capable of “synergis-ing” information from within and without, “vibrational medicine” such as homoeopathic remedies and crystal/flower essences are messages contained within the coherent structure of water molecules, these coherences having been encouraged and strengthened by the practices used in their production.”
I believe that it is serendipitous that both the importance of gut bacteria to the function of the immune system, and the true function of the appendix in informing the nature of the bacteria required, has become extant coincident with the recent pandemics (and conventional medicine’s Frankensteinian attempts to control its off-springs), quote; "Most of the microbes in your intestines are found in a “pocket” of your large intestine called the cecum, and they are referred to as the gut microbiome.
Although many different types of microbes live inside you, bacteria are the most studied.
In fact, there are more bacterial cells in your body than human cells. There are roughly 40 trillion bacterial cells in your body and only 30 trillion human cells. That means you are more bacteria than human (1Trusted Source, 2Trusted Source).
What’s more, there are up to 1,000 species of bacteria in the human gut microbiome, and each of them plays a different role in your body. Most of them are extremely important for your health, while others may cause disease (3Trusted Source).
Humans have evolved to live with microbes for millions of years.
During this time, microbes have learned to play very important roles in the human body. In fact, without the gut microbiome, it would be very difficult to survive.
The gut microbiome begins to affect your body the moment you are born.
You are first exposed to microbes when you pass through your mother’s birth canal. However, new evidence suggests that babies may come in contact with some microbes while inside the womb (4Trusted Source, 5Trusted Source, 6Trusted Source).
As you grow, your gut microbiome begins to diversify, meaning it starts to contain many different types of microbial species. Higher microbiome diversity is considered good for your health (7Trusted Source).
Interestingly, the food you eat affects the diversity of your gut bacteria.
As your microbiome grows, it affects your body in a number of ways, including:
Digesting breast milk: Some of the bacteria that first begin to grow inside babies’ intestines are called Bifidobacteria. They digest the healthy sugars in breast milk that are important for growth (8Trusted Source, 9Trusted Source, 10Trusted Source).
Digesting fiber: Certain bacteria digest fiber, producing short-chain fatty acids, which are important for gut health. Fiber may help prevent weight gain, diabetes, heart disease and the risk of cancer (11Trusted Source, 12Trusted Source, 13Trusted Source, 14Trusted Source, 15Trusted Source, 16Trusted Source, 17Trusted Source).
Helping control your immune system: The gut microbiome also controls how your immune system works. By communicating with immune cells, the gut microbiome can control how your body responds to infection (18Trusted Source, 19Trusted Source).
Helping control brain health: New research suggests that the gut microbiome may also affect the central nervous system, which controls brain function (20Trusted Source)." Why the Gut Microbiome Is Crucial for Your Health
“Microbiome refers to the collective genomes of the micro-organisms in a particular environment, and microbiota is the community of micro-organisms themselves (box 1). Approximately 100 trillion micro-organisms (most of them bacteria, but also viruses, fungi, and protozoa) exist in the human gastrointestinal tract12—the microbiome is now best thought of as a virtual organ of the body. The human genome consists of about 23 000 genes, whereas the microbiome encodes over three million genes producing thousands of metabolites*, which replace many of the functions of the host,13 consequently influencing the host’s fitness, phenotype, and health.2”…
"win studies have shown that, although there is a heritable component to gut microbiota, environmental factors related to diet, drugs, and anthropometric measures are larger determinants of microbiota composition.45
Gut microbes are key to many aspects of human health including immune,6 metabolic5 and neurobehavioural traits (fig 1).78 Different levels of evidence support the role of gut microbiota in human health, from animal models910 and human studies.4111213"…
"What does the gut microbiota do?
The gut microbiota provides essential capacities for the fermentation of non-digestible substrates like dietary fibres and endogenous intestinal mucus. This fermentation supports the growth of specialist microbes that produce short chain fatty acids (SCFAs) and gases.17 The major SCFAs produced are acetate, propionate, and butyrate.
Butyrate is the main energy source for human colonocytes, can induce apoptosis of colon cancer cells, and can activate intestinal gluconeogenesis, having beneficial effects on glucose and energy homeostasis.18 Butyrate is essential for epithelial cells to consume large amounts of oxygen through β oxidation, generating a state of hypoxia that maintains oxygen balance in the gut, preventing gut microbiota dysbiosis.19
Propionate is transferred to the liver, where it regulates gluconeogenesis and satiety signalling through interaction with the gut fatty acid receptors 18 Acetate—the most abundant SCFA and an essential metabolite for the growth of other bacteria—reaches the peripheral tissues where it is used in cholesterol metabolism and lipogenesis, and may play a role in central appetite regulation.20 Randomised controlled trials have shown that higher production of SCFAs correlates with lower diet-induced obesity21 and with reduced insulin resistance.22 Butyrate and propionate, but not acetate, seem to control gut hormones and reduce appetite and food intake in mice.21 Gut microbial enzymes contribute to bile acid metabolism, generating unconjugated and secondary bile acids that act as signalling molecules and metabolic regulators to influence important host pathways.23
Other specific products of the gut microbiota have been implicated directly in human health outcomes. Examples include trimethylamine and indolepropionic acid. The production of trimethylamine from dietary phosphatidylcholine and carnitine (from meat and dairy) depends on the gut microbiota and thus its amount in blood varies between people. Trimethylamine is oxidised in the liver to trimethylamine N-oxide, which is positively associated with an increased risk of atherosclerosis and major adverse cardiovascular events.24 Indolepropionic acid is highly correlated with dietary fibre intake25 and has potent radical scavenging activity in vitro,26 which seems to reduce the risk of incidence of type 2 diabetes.25" https://www.bmj.com/content/361/bmj.k2179
*Italics mine.
Now let’s look at the role of the (useless; “throw it away” -also re: tonsils-), appendix…
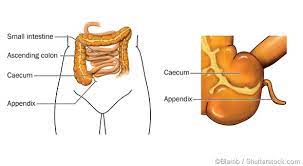
Quote; "A growing body of research suggests that the appendix, far from being useless, has a real function in the digestive system. The prevailing view of the appendix began evolving in the past decade, as researchers learned more about the complicated interactions between the body and the microbial ecosystem inside the intestines. As the importance of gut bacteria became clearer, researchers realized that the appendix, partially isolated from the digestive system, served as a refuge for helpful bacteria during bouts of intestinal illness. Once the disease cleared, helpful microbes from the appendix could repopulate the gut.
Formally known as the vermiform (worm-shaped) appendix, the appendix is located behind or below the cecum, the very beginning portion of the large intestine. Infections of the appendix (appendicitis) can be fatal, and have been described in scholarly papers for more than a hundred years. Appendectomies have been performed for even longer.
Unable to discern its function, physicians and scientists assumed that the appendix was a useless holdover of the evolutionary past."…
“The less fanciful literature focuses mostly on one well-known phenomenon: that removing the appendix seems to be an effective treatment for certain forms of ulcerative colitis. To date, nobody understands why, and even before the new research, doctors did not advocate removing the appendix as a preventative measure. And this recent scholarship describes a special immune response specific to the appendix, suggesting that the body considers it well-worth defending*.” Appendix May Actually Have a Purpose
*Italics mine.
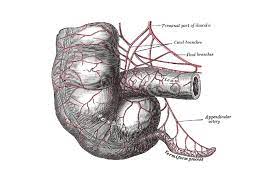
Quote; "This literature review assesses the current knowledge about the immunological aspects of the vermiform appendix in health and disease. An essential part of its immunological function is the interaction with the intestinal bacteria, a trait shown to be preserved during its evolution. The existence of the appendiceal biofilm in particular has proved to have a beneficial effect for the entire gut. In assessing the influence of acute appendicitis and the importance of a normally functioning gut flora, however, multiple immunological aspects point towards the appendix as a priming site for ulcerative colitis. Describing the immunological and microbiotical changes in the appendix during acute and chronic inflammation of the appendix, this review suggests that this association becomes increasingly plausible. Sustained by the distinct composition of cells, molecules and microbiota, as well as by the ever more likely negative correlation between the appendix and ulcerative colitis, the idea of the appendix being a vestigial organ should therefore be discarded.
Introduction
Until recently, the human appendix has been regarded as a rudimentary part of the intestine. During the past few years, however, several studies have suggested its immunological importance for the development and preservation of the intestinal immune system 1. The appendix has been shown to have an important interaction with the intestinal flora 2, 3, 4. Considering the appendix as a ‘safe house’ for the commensal gut flora, these studies hypothesize that commensal bacteria can be reintroduced from the appendix in case of disease, and therefore the appendix can be considered as an important part of intestinal health. This literature review assesses the current knowledge concerning the immunological aspects of the vermiform appendix. By describing its normal physiology and the importance of its biofilm, and appraising its evolution and elucidating which aspects have changed or, more importantly, which have been preserved in the long history of its existence, a clearer understanding of its influence on the intestinal immune system will be provided." The immunology of the vermiform appendix: a review of the literature - PMC
I contend that informative as these articles are they represent tentative “baby-steps” by conventional physicians into the truly wondrous (and vast), subject of the functioning of the human endocrine system. I also contend that it is via the interaction between the endocrine system and the organs of the stomach (incl. the appendix), that much of the “messaging” from vibrational medicines informs the host (patient).
“Physicians who are not themselves physicists treat physicists who are not themselves physicians and are informed by same!”
All physicians should know that the most important principle in medicine is to maintain an open and honest relationship between doctor and patient.